Perspectives on Medical Reimbursement
By JR Associates
The path to advancements in disease detection and treatment is notoriously complex, circuitous and costly. However, even after FDA approval, there are no guarantees of reimbursement through CMS coverage.
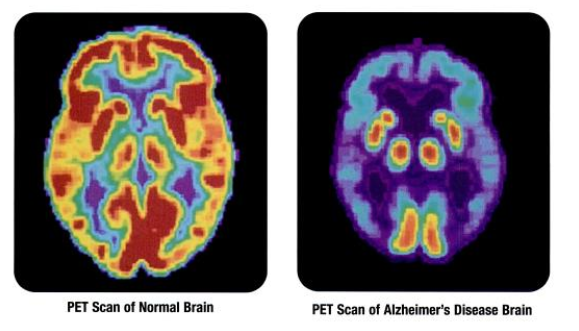
This is an essential lesson in the case of Eli Lilly’s Amyvid PET scan imaging agent, which is used to detect amyloid plaques in the diagnosis of Alzheimer’s Disease (AD) and other cognitive disorders.
As explained in a recent Medical Device Daily article, detection of amyloid brain plaques is integral to the AD diagnostic process. Currently, the standard for Medicare coverage is tied to FDG-PET. However, in January, CMS will consider coverage evidence and implications in the use of Lilly’s Amyvid as an alternative.
Interestingly, in “CMS Eyes PET Coverage for Detection of Amyloid Plaques,” MDD Washington Editor, Mark McCarty, explains that Lilly actually doesn’t support use of the imaging agent “to establish a diagnosis” or to monitor therapeutic progress. Instead, the test is “seemingly … intended to rule out diseases as much as to confirm them.”
JR Associates Vice President of Global Health Policy, Jo Ellen Slurzberg, outlined multiple implications for McCarty:
• This scenario is unusual because “Medicare doesn’t traditionally cover rule-out diagnostics.”
• Lilly may be unable to expand its coverage definition, because FDA approval was based on a study where “indication for use is very specific.”
• There is a possibility that demand could surge in response to patient expectations. In other words, if people ask doctors to rule-out Alzheimer’s as the cause of any cognitive decline, the volume of PET scans could soar – especially as the aging population increases.
The stakes are high for Lilly, given the tremendous market potential for Amyvid. According to Alzheimer’s Association statistics in The RPM Report, there are currently 5.4 million cases of AD in the U.S. That number is expected to triple by 2050, with 1 million new cases expected each year thereafter. “And, as a test to support diagnosis, Amyvid could be used in the much broader population of those over 65 showing signs of dementia.”
At the January Medicare Coverage and Advisory Committee (MedCAC) meeting, it is likely that CMS will seek advice about how best to manage this technology and assure appropriate use. More importantly, if the evidence demonstrates improved outcomes, it is unlikely that CMS will make a final decision until sometime after the meeting takes place.
Is your organization seeking a more effective reimbursement strategy? Contact us anytime to schedule preliminary consultation. Call us at 1-818-344-4380 or send us an email at info@1jra.com.
• Learn more about our comprehensive reimbursement services
• Read more articles by and about our consultants
• Visit our Newsroom for more updates and industry alerts









